Let’s talk about pain
Pain is an important sensory experience to aid our survival. We know that in rare cases where an individual is unable to experience pain, they live a shorter life as they are unable to respond quickly to hazards.
So what is pain and how does it work?
Throughout our body, we have nerve receptors to detect various sensations such as temperature, vibration, pressure etc. These receptor messages travel up to the brain via the spinal cord. Many complex interactions occur along this pathway in the spinal cord and throughout the brain. We see on MRI scanning, that when a certain body part is exposed to a noxious stimulus such as heat or cold, the brain lights up in a particular pattern (Figure 1). This indicates that the parts of the brain involved in the majority of people represent a fairly healthy response to the stimulus. The situation is different in people with chronic pain, and we will discuss this in a moment.

Figure 1: A diagrammatic example of a brain ‘neurotag’ for pain – the brain activation pathway for a particular pain experience. This fires in descending order from 9 (spinal cord) to 1 (brain cortex), but in a chronic pain state it can be activated or ‘turned on’ by any number as well as additional factors. Credit to Advanced Physical Therapy https://advance-physicaltherapy.com/2015/science-helps-understand/
Let’s look at the definition of pain from the IASP -International Association for the Study of Pain1,2
“Pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”
So let’s talk about ‘actual or potential’…. This means that a person can experience pain, even when there is nothing touching that body part, but they might perceive a threat of damage/ pain which triggers the pain response. We’ll discuss this in the next section.
The IASP definition is expanded upon by the addition of six key notes and the etymology of the word pain for further valuable context.
- Pain is always a personal experience that is influenced to varying degrees by biological, psychological, and social factors.
- Pain and nociception are different phenomena. Pain cannot be inferred solely from activity in sensory neurons (this means that your pain experience is not related to what is happening in your sensory nerve endings throughout your body and is impacted by other things e.g. memory, fear, stress)
- Through their life experiences, individuals learn the concept of pain.
- A person’s report of an experience as pain should be respected (the person’s pain experience is theirs alone and should be respected even if it doesn’t make sense to you. Their experience is their experience. It doesn’t make sense to most scientists but this is changing and the world is starting to understand a bit more about pain and how it operates).
- Although pain usually serves an adaptive role, it may have adverse effects on function and social and psychological well-being. (so although it is there to protect us, it can become overprotective in the case of chronic pain and may inhibit our desire or confidence to perform our usual activities)
- Verbal description is only one of several behaviours to express pain; inability to communicate does not negate the possibility that a human or a nonhuman animal experiences pain. (It is often very difficult for people to understand and describe what they are feeling. Your skills in observing behaviours may alert you).
What is chronic pain?
Chronic pain, also known as ‘persistent’ pain, is where a pain experience continues for 3 months or more.
In these situations, the pain processing pathways begin to change. Pain processing may become more complex, have a larger response to stimuli and incorporate more areas in the brain.
In addition, the pain pathway can often be activated by non-physical stimuli, for example just thinking about another person or activity may activate the ‘feeling of pain’ that a person experiences, or even being in a thunderstorm if that is when the initial injury occurred.
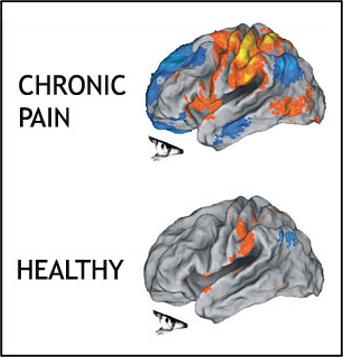
Figure 2: The image shows widespread activation of the brain cortex in people with chronic pain, compared to healthy asymptomatic subjects. Credit: Northwestern University referenced by Physio-paedia3
In the chronic or persistent pain stage, the psychosocial factors can become strong ‘ignition cues’ that can activate pain. These psychosocial factors have usually been present since the time of injury and gradually, or rapidly, worsen over time. This is why it is so important to try to identify very early on all factors that are worrying the person and to resolve these issues as soon as possible, so that they do not increase pain, decrease function and become barriers to long term recovery and return to work and life.
Why do people develop chronic pain?
We don’t know. But we do know that the following factors can increase the likelihood of chronic pain:
- Fear
- Anxiety and depression
- Previous injuries
- Experiences of those around them
- General health – diabetes, other systemic conditions
- Poor sleeping patterns
- Smoking history
- Cultural experience
- Previous abuse
- PTSD
- Perceived low home support – Personal stress – relationships, family, financial
- Perceived low workplace support – important to aim for easy collaborative conversation with managers and work team
- Difficulty communicating – personal communication style, language barriers
- RTW team stress – team members not working together, having opposing goals, poor communication etc.
So what can we do to help?
Prevention:
- Best outcomes are achieved with early identification of factors that place the person at a higher risk of developing chronic pain and having a delayed return to work. We encourage health providers to screen patients using the Orebro Musculoskeletal Pain Questionnaire to identify the risk of a delayed recovery as well as to assist in identifying underlying factors and concerns that should be addressed quickly. According to a recent study in Australia, overall claim costs were reduced by 30% when this approach was taken4 .
- If a person is identified as at risk of a delayed recovery, early referral to a psychologist or low intensity mental health coach is a critical factor in achieving an earlier return to work and life4. This early psychological intervention enables the person to learn strategies to help them manage and overcome potential barriers to recovery.
- Another important component of prevention is to work collaboratively with the person and empowering them to ensure that they are actively contributing to the planning, execution and evaluation of their recovery and return to work.
Treatment: Can pain be treated?
In short, yes it can (in most cases). We know that various approaches can help to reduce pain or resolve it all together.
This usually involves good quality pain education (learning about how pain works and how to reduce it), which has been found to result in ongoing improvements well after the education sessions (Figure 3). Treatment also involves movement re-education and rehearsal, graded return to activity, relaxation techniques and pacing tasks, reviewing and practicing tasks at the workplace, working with the employer, worker, allied health practitioner and claims manager onsite regularly. It may include other aspects including cognitive retraining with apps and other exercises, exercise and strengthening programs, and many other interventions.
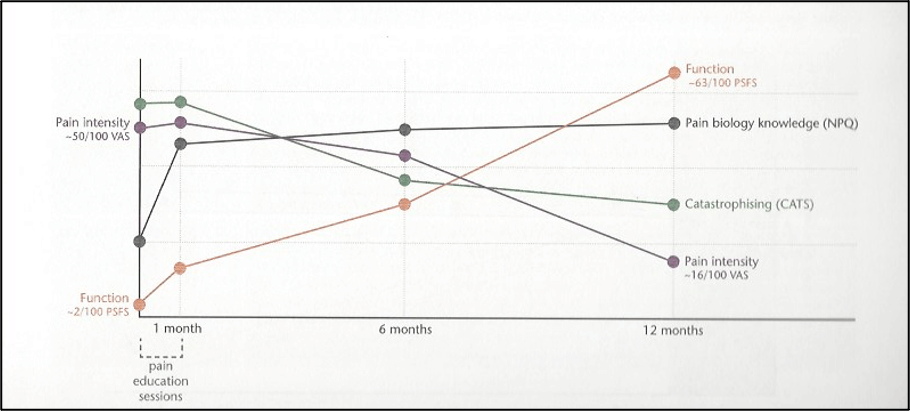
Figure 3: The impact of 1 month of ‘Explain Pain’ pain education program over time on pain biology knowledge, catastrophising and pain intensity. Continued improvements are seen in all areas across the following 12 month period.5
Pain is also described as the balance between perceived danger and perceived safety. This is explored in detail in resources such as ‘The Explain Pain Handbook: Protectometer’6 which I will briefly summarise here.
The more danger that the person feels they are in, the higher the pain levels (perceived threat or danger, ‘Danger In Me’ = ‘DIM’). The safer the person feels, the lower the pain levels (perceived safety, ‘Safety In Me’ = ‘SIM’).
Identifying the factors that turn the pain up (DIMs) or turn the pain down (SIMs) and resolving these issues, can significantly reduce pain and improve function. Health providers will talk to the patient to identify these factors and may introduce new concepts to increase the SIMS and decrease the DIMS. Figure 4 (see the Explain Pain Handbook: The Protectometer6).

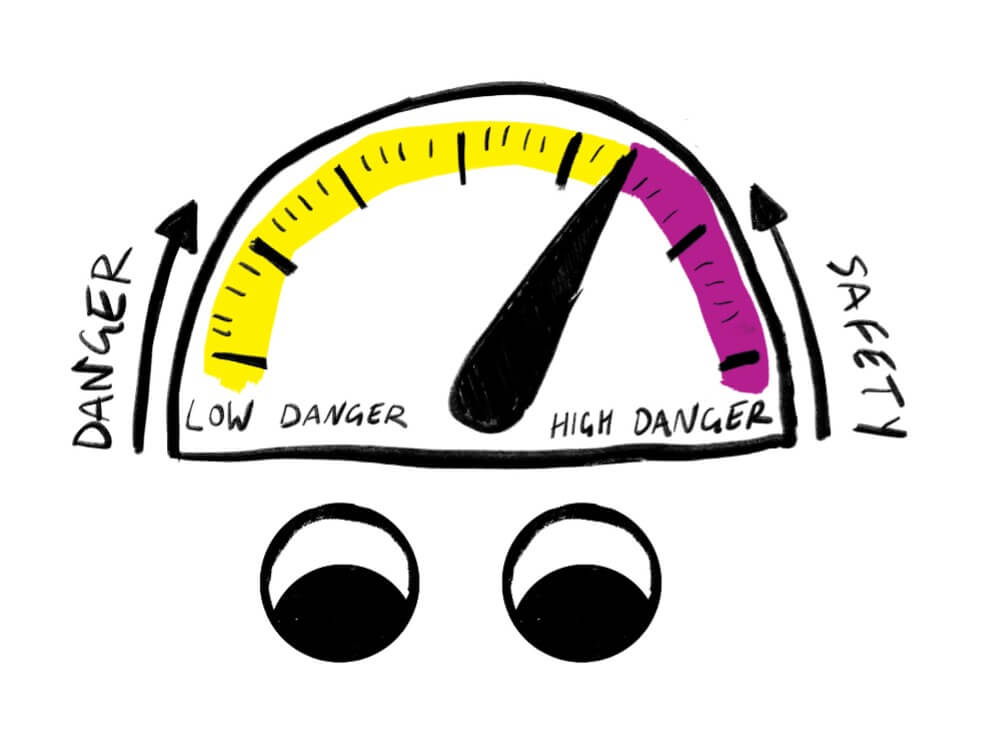
Figure 4 a and b: a) a pain scale example, and; b) understanding the threat of danger versus safety and the impact on pain. Health providers investigate with the person what turns the pain up (perceived threat or danger, ‘Danger In Me’ = ‘DIM’) and what turns the pain down (Perceived safety, ‘Safety In Me’ = ‘SIM’). Treatment will assist the person to understand these factors and increase the number of SIMS, whilst decreasing the number of DIMS to ‘turn the pain down’ and improve recovery. Acknowledgement for X(b) to the Neuro-Orthopaedic Institute and ‘The Explain Pain Handbook: Protectometer’6.
It is important to set goals with associated timelines, work with the person and treating team and regularly review that the person is progressing with the selected form of treatment. If not, do they need a few weeks more of that treatment type, or is it time to consider other options? Discuss this with the patient and treaters to ensure that the person is receiving the best possible treatment and impact.
Where do I go for more information?
There is a lot of information out there, but what is reliable and trustworthy?
- Check out the Pain Revolution website for reliable, informative fact sheets. This group is from our internationally renowned UniSA team, Body in Mind. https://www.painrevolution.org/factsheets
- Also, this link might be helpful to share with your workers if you feel appropriate:
https://youtu.be/24P7cTQjsVM
[1] IASP – International Association for the Study of Pain Task Force 2020. https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
[2] Raja, Srinivasa N; Carr, Daniel B; Cohen, Milton; Finnerup, Nanna B; Flor, Herta; Gibson, Stephen; Keefe, Francis J; Mogil, Jeffrey ; Ringkamp, Matthias; Sluka, Kathleen A; Song, Xue-Jun; Stevens, Bonnie; Sullivan, Mark D; Tutelman, Perri R; Ushida, Takahiro; Vader, Kyle (2020) The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain 161(9): 1976-1982. DOI: 10.1097/j.pain.0000000000001939. https://journals.lww.com/pain/Citation/2020/09000/The_revised_International_Association_for_the.6.aspx
[3] https://www.physio-pedia.com/Chronic_Pain_and_the_Brain
[4] Nicholas MK, Costa DSJ, Lindon SJ, Main CJ, Shaw WS, Pearce G, Gleeson M, Pinto RZ, Blyth FM, McAuley JH, Smeets RJEM and McGarity A (2020) Implementation of Early Intervention Protocol in Australia for ‘High Risk’ Injured Workers is Associated with Fewer Lost Work Days Over 2 Years Than Usual (Stepped) Care. J.Occ.Rehab. 30:93–104. https://doi.org/10.1007/s10926-019-09849-y
[5] Lee H, McAuley JH, Hubscher M, Kamper SJ, Traeger AC and Moseley GL (2016) Does changing pain-related knowledge reduce pain and improve function through changes in catastrophizing? Pain 157: 922-930. http://dx.doi.org/10.1097/j.pain.0000000000000472
[6] Moseley GL and Butler DS (2015) The Explain Pain Handbook: Protectometer. Neuro Orthopaedic Institute & Noigroup Publications, Adelaide Australia.
Dr Cassandra Zaina FACP ReturnToWorkSA Physiotherapy Advisor, Scheme Support
Version: 26 January 2023.